The Less-talked-about Effects of Breast Cancer Treatment

By Robert Donati, PT, CLT, Aquacare Physical Therapy
This is the second part of a 2-part series on breast cancer diagnosis and its outcomes.
When we talk about breast cancer we may think about pink ribbons, or about the testing leading to diagnosis, staging, radiation, chemotherapy, and surgical procedures.
However, while breast cancer is a life-changing diagnosis, often the biggest changes in patients’ lives don’t come until after treatment.
Some of the side effects of “curing the cancer” are radiation burns, cording, and secondary lymphedema, or lymphedema caused by trauma to tissue.
Injury Following Breast Cancer Treatment
Radiation is the use of x-rays and other high-energy rays to kill or destroy abnormal cells. It can cause damage to normal cells in addition to killing the cancer cells. This results in radiation burns, causing pain and also decreased tissue elasticity when healing occurs. The treatment is skin care and gentle range-of-motion exercises, including stretching and scar releases to increase the tissue pliability and increase functional motion for the extremity.
Muscle cording is another possible side effect from the treatment of breast cancer. It usually can start in a very short period of time after the surgery.
Cording – also known as axillary web syndrome (AWS) – is a side effect of having lymph nodes removed as a result of breast cancer. A cord, or web of cords, develops under the skin on the inside of your arm. This cording leads to tightness which can extend from the scar site down the arm to the elbow and in some cases, across the forearm.
In extreme cases, it can also spread from the axilla to the chest wall.
The treatment is usually performed by a physical or occupational therapist who specializes in the treatment of post operative patients. Your therapist may start treatment by gently trying to release the cord by pulling on the tissue of the outstretched arm and working from the axilla to the wrist. Sometimes when the treatment works patients will feel a snapping in the tissue as it is released. Performing gentle stretches immediately after the surgery can reduce the possibility of cording occurring.
Secondary lymphedema is the most problematic side effect of breast cancer surgical intervention. This is the accumulation of protein rich fluid in the tissue of the traumatized area and can occur in any area of the body including the head, neck, arms, legs, genitals, and trunk.
Approximately 30% of patients will develop lymphedema though the statistics range from 2-83% incidence of an adverse occurrence. There are no diagnostic tests that check for lymphedema, so the only way to be diagnosed is through a complete medical history, physical exam, and review of risk factors for lymphedema.
Some risk factors include treatment history, having an active cancer diagnosis, or having experienced trauma to the body part at risk for lymphedema.
Symptoms of Undiagnosed Lymphedema
Often, lymphedema goes undiagnosed because symptoms can be so mild that the patients do not report them to their surgeon.
Some of those symptoms include:
- Heaviness
- Tightness
- Firmness
- Pain/aching/soreness
- Numbness
- Tingling
- Stiffness
- Limb fatigue or limb weakness.
There are four stages of lymphedema:
- Stage 0 is characterized by a limb that is normal but has decreased lymphatic flow.
- Stage 1 is denoted by swelling that resolves with elevation of the limb.
- Stage 2 has pitting edema that does not resolve with elevation.
- Stage 3 is categorized by changes in the skin including hyperpigmentation, hyperkeratosis, hyperplasia, papillomatosis, lymphorrhea, and or elephantitis.
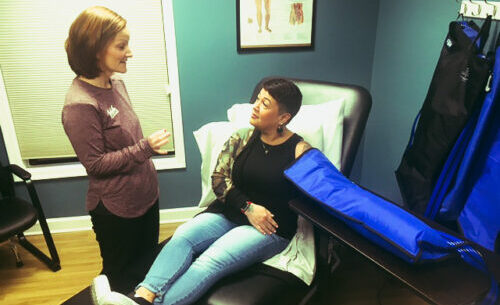
The “gold standard” of treatment for lymphedema is Complete Decongestive Therapy (CDT). This treatment plan consists of skin care, education, manual lymph drainage, multilayer gradient compression wraps, decongestive exercises, and vasopneumatic compression pumps for the affected extremity or body part.
Treatment usually occurs in two phases. During the first phase, patients work with a certified lymphedema therapist at a physical therapy practice. Then, phase two allows the patient to continue treatment at home through exercises, compression garments, massage, or other techniques to keep the lymphedema swelling under control.
While lymphedema can be managed through physical therapy and management techniques, there are surgical options. These can include vascular lymph node transfer where the physician will take a healthy lymph node and place it in the problematic area.
A second option is lymphovenous bypass when the surgeon connects lymphatic vessels to nearby small veins. One benefit of this procedure is it can be performed as an outpatient and has minimal incisions and blood loss.
A third more-invasive option is the Charles procedure where skin is removed and grafted into the affected areas to repair them.
There are many other issues that can result from the surgical or non-surgical treatments for breast cancer, but know that you are not alone.
Your physical or occupational therapist will be with you every step of the way to help you recover from your surgery and advance on the road to recovery from breast cancer.
Aquacare Physical Therapy has one of the largest teams of certified lymphedema therapists in the region with locations in Seaford, Milford, and Lewes, Delaware, and Easton and Salisbury, Maryland.
Call the Aquacare office closest to you, call the Seaford office at 302-536-1774 or schedule your appointment online: www.aquacarephysicaltherapy.com.