Guide to Breast Cancer Surgery Recovery

By Robert F.Donati, PT, CLT
This is Part One of a 2-part series on breast cancer diagnosis and outcomes, including returning to pre-cancer activities.
October has been designated as breast cancer awareness month for the last four decades and has been signified with the use of the pink ribbon to bring attention to breast cancer. Each year there are over 240,000 women diagnosed with breast cancer. That is 1 in 8 women or 13% of all women. And, 80% of those diagnosed are over the age of 45.
There are many treatment options when diagnosed with breast cancer, some non-surgical and others surgical. Non-surgical treatments are employed when cancers are too large to be removed without the ability to leave healthy tissue at the margins. Some options for treatment include Teletherapy which is a form of radiation therapy that uses x-rays and other high energy rays to kill or destroy abnormal cells, chemotherapy, immunotherapy, targeted therapy, or hormonal therapy. Neoadjuvant chemotherapy may also be performed with the intent of reducing the size of the breast cancer tumor, making surgery a more appropriate option.
Surgical options include Breast Conservation Surgery (BCS) or mastectomy. The goal of BCS is to leave behind as much normal breast tissue as possible and is sometimes also called a wide local excision or lumpectomy. The combination of BCS and radiation therapy is called breast conserving therapy or BCT and consists of lumpectomy, sentinel node biopsy, or possible axillary dissection and may have similar overall long-term survival rates of mastectomy in patients with early stage cancer.
Another procedure performed is the mastectomy. There are many variations and each is depending on the amount of tissue spared by the surgeon. With the simple mastectomy, the surgeon removes the entire breast, including the nipple, areola, and covers the entire pectorals muscle, skin, and a couple of lymph nodes from the underarm or sentinel lymph node biopsy. A modified radical mastectomy combines a simple mastectomy with removal of the lymph nodes under the arm or axillary dissection. Finally, during the least common procedure, radical mastectomy, the surgeon removes the entire breast, underarm lymph nodes, and the chest wall muscles under the breast. The last two types of mastectomy are the skin-sparing and nipple-sparing mastectomy. During skin-sparing mastectomy, breast tissue, nipple and areola are removed and with the nipple-sparing surgery, the nipple and areola are left intact. There is one additional surgery, a double mastectomy and sometimes it is performed as a preventative surgery for women who are at risk for developing breast cancer.
After mastectomy, women may opt for breast reconstruction surgery. The two main types are implant reconstruction and flap reconstruction. Implant surgery avoids more extensive surgery and does not use tissue from another part of the body. Either during or at a time after the surgery there is a tissue expander placed under the pectoral or chest muscle to stretch tissue over a period of time, to create a pocket for the implant. This is done by having a port where saline can be injected at slow intervals until the skin and tissue is stretched to appropriate lengths. An implant can then be placed, completing the reconstruction process.
The second procedure is the flap reconstruction using the tissue, including skin, fat, and sometimes muscle from another part of the body to reconstruct the breast. This allows for a natural appearance of the breast as compared to implants. The drawback of the procedure is that there will be a scar from the incision on the tummy.
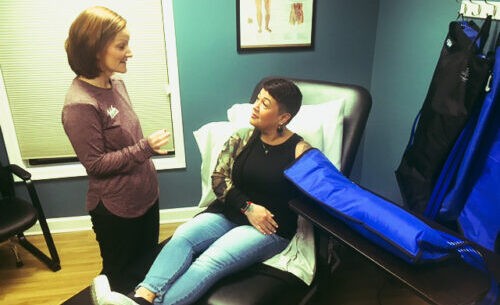
After surgery, there is the possibility of developing limitations in range of motion (ROM), strength, and functional mobility. The key is early mobilization and activity. After surgery, patients may be referred to a specialist who may be either a physical or occupational therapist to reduce pain, increase range of motion, increase strength, and normalize functional mobility.
These can all be achieved with gentle and progressive manual and self stretching and strengthening exercises when healing post surgical healing allows including scar massage, posture stretching, Complete Decongestive Treatment (CDT), and ROM in pain-free planes (including active, active assisted, and passive ROM) of the affected body parts.
Treatment will be determined after an initial evaluation with a physical or occupational therapist who will then determine the treatment that will best address the needs found on the first treatment.
Aquacare Physical Therapy has one of the largest teams of certified lymphedema therapists in the region with locations in Seaford, Milford, and Lewes, Delaware, and Easton and Salisbury, Maryland.
Call the Aquacare office closest to you, call the Seaford office at 302-536-1774 or schedule your appointment online: www.aquacarephysicaltherapy.com.