
Dry Needling For Neck Pain


Many people elevate or round their shoulders causing tightness in the supporting muscles. Many people also have very tight upper trap muscles leading to multiple problems – Headaches, pain, poor posture, difficulty raising arms overhead…the list could go on. “These are common complaints heard by physical therapists. Patients often ask what can be done to cure or fix the problem.
Unfortunately, there is no cure, however there are many options that can be used to help reduce pain, improve posture and release muscular tension. One treatment option available is Dry Needling (DN).
DN uses a thin filament needle that is inserted into the dysfunctional tissue (muscle spasm /myofascial dysfunction) and is then moved up/down to facilitate a twitch response to release the muscular spasm. Some people will get immediate relief and may not need additional treatment.
Your physical therapist will be able to address and get to the root of the problem to assess if further sessions may be needed. Following DN you may be asked to perform some light stretching and/or gentle movement of the neck to assist with maintaining mobility. Ice and heat are also encouraged to reduce the soreness that may follow. Get to your local physical therapist and see if Dry Needling may be appropriate for you!
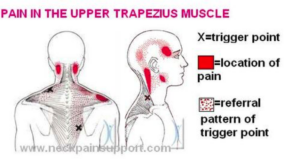
Myofascial Dysfunction or Myofascial Pain Syndrome is another name for muscle pain. This is a chronic condition involving inflammation within the connective tissue. Symptoms may include deep muscle ache/pain, pain that does not go away and/or pain that continues to persist for a period of time. Myofascial dysfunction has been around for hundreds of years with the onset of trigger points (hyper sensitive spots) within muscles -also being termed muscular spasms around 1938. Dry needling became more prominent as a treatment amongst physical therapist in 2006. You must check with your local physical therapist or physical therapy state boards to see if your state allows for DN to be practiced within the scope of the state’s practice act.
Aquacare Physical Therapy in Millville, DE can assist you with reduction of pain and helping you regain functional movement. Please call for a free consultation or to set up an initial evaluation.
https://aquacarephysicaltherapy.com/schedule-an-evaluation/