Physical Therapy for Bowel Disorders

By Cara Konlian, MSPT, CEO, Aquacare Physical Therapy
Most people are unaware that pelvic floor therapy can help in the management of bowel disorders.
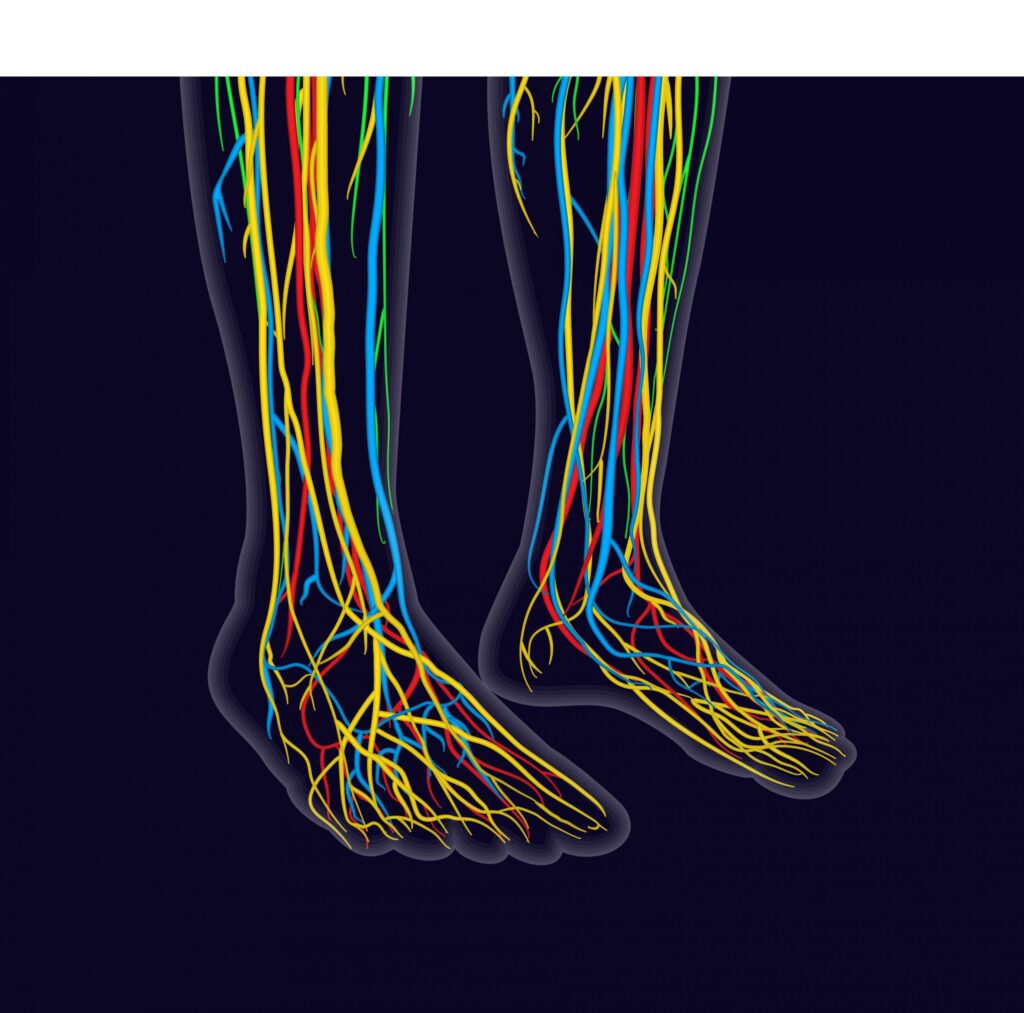
Physical therapists can evaluate and treat the musculoskeletal and neuromuscular components of bowel dysfunction in order to improve a patient’s quality of life.
Some bowel disorders proven to improve with physical therapy include:
- Fecal Incontinence
- Bowel Frequency, Urgency, Retention, and/or Incomplete Emptying
- Flatulence
- Diarrhea
- Constipation
- Rectocele
- Abdominal Bloating
- Anal/Rectal and/or Abdominal Pain, Pressure, or Spasm
Musculoskeletal dysfunctions can be treated using techniques such as releasing myofascial trigger points in the abdomen, back, gluteal, and pelvic floor; neuromuscular re-education; and strengthening of the muscle groups.
Causes and treatment for constipation
Constipation is a common disorder that primary care physicians and gastroenterologists diagnose on a regular basis.
There are many causes of constipation. It can be a motility and gut transit issue, or it may be pelvic floor dyssynergia, meaning the pelvic floor muscles fail to relax and contract properly. The pelvic floor is a group of muscles at the base of the pelvis that help control sexual, urinary, and bowel function.
These muscles must relax and contract properly to maintain urinary and fecal continence, sexual function and proper voiding habits.
The inability to relax and contract the pelvic floor muscles correctly can lead to symptoms of constipation, straining with bowel movements, and feelings of incomplete evacuation.
Causes and treatment of diarrhea
Diarrhea is defined as a condition in which feces are discharged from the bowels frequently and in a liquid form. Leakage from diarrhea can occur due to weak pelvic floor muscles.
Physical therapists trained in the dysfunctions of pelvic floor and bowels can help you regain control over these muscles and reduce issues caused by diarrhea.
Causes and treatment of Irritable Bowel Syndrome (IBS)
Signs and symptoms of IBS may include abdominal pain or discomfort, bloating, gas, frequent bowel movements, diarrhea, or constipation. As one of the most common disorders of the gastrointestinal system, IBS may cause tightening, weakening, or incoordination of the pelvic floor and abdominal musculature.
With a personalized physical therapy and pelvic floor treatment plan, your muscle strength will improve and many IBS symptoms can be resolved.
Causes and treatment of fecal incontinence
Fecal incontinence is the inability to control bowel movements, causing stool to leak unexpectedly. Precursor symptoms include soiling, fecal urgency, and flatulence. The amount of stool will vary as sometimes only a small quantity will be lost or the complete bowel movement may be lost.
Fecal Incontinence can occur due to the following:
- Muscle damage. Injury to the rings of muscle at the end of the rectum (anal sphincter) may make it difficult to hold stool back properly. This kind of damage can occur during childbirth, especially if you have an episiotomy or forceps are used during delivery.
- Nerve damage. Injury to the nerves that sense stool in the rectum or those that control the anal sphincter can lead to fecal incontinence. The nerve damage can be caused by childbirth, constant straining during bowel movements, spinal cord injury or stroke. Some diseases, such as diabetes and multiple sclerosis, also can affect these nerves and cause damage that leads to fecal incontinence.
- Loss of storage capacity in the rectum. Normally, the rectum stretches to accommodate stool. If your rectum is scarred or your rectal walls have stiffened from surgery, radiation treatment or inflammatory bowel disease, the rectum can’t stretch as much as it needs to, and excess stool can leak out.
Causes and treatment of hemorrhoid pain
Hemorrhoids are painful, swollen, and inflamed veins around the anus and rectum. They occur usually due to straining with bowel movements with pregnancy or chronic constipation.
Hemorrhoids can be external (skin around the anus) or internal (inside the anal canal). If the muscles or tissues in the rectum and anal canal are restricted or in spasm, blood flow to the hemorrhoid is restricted. This decreased circulation can make healing more difficult.
Physical therapy can help increase tissue mobility and reduce muscle spasms in the affected area.
Causes and treatment of rectocele (protrusion)
A rectocele is the protrusion of rectal tissue in the posterior vaginal wall. It may occur with childbirth, chronic constipation, chronic coughing, heavy lifting, estrogen deficiency, abdominal weakness, and obesity.
Symptoms may include constipation or pelvic pain, and fecal or urinary incontinence.
A rectocele may be prevented through correct body mechanics with lifting, avoidance of straining, controlling, and treating constipation, weight control, core-stabilization exercises, and Kegels.
A rectocele can be successfully managed through pelvic floor physical therapy.
Physical therapy for bowel disorders
Some of the physical therapy treatments for bowel disorders include external and internal rectal myofascial release techniques, trigger point release techniques, biofeedback therapy to help down-train tight muscles or up-train weak muscles, instruction to correct bowel techniques to prevent straining, instruction in-home exercise program to stretch and strengthen the pelvic floor, hip, and gluteal muscles.
Manual therapy is needed to reduce the tension, adhesions, and knots in muscles that cause them to become dysfunctional.
Biofeedback therapy helps re-train the pelvic floor muscles’ ability to contract and relax within their full range of motion. It is a treatment that requires either the insertion of a rectal sensor (sensor is the size and length of a pinky) or external sensors to measure pelvic floor muscle tension through electromyography (EMG).
The EMG activity is visually displayed on the biofeedback unit so a patient can see what their muscles are doing and learn to better control these muscles with verbal and tactile cueing from the physical therapist. Identifying the internal sensations associated with relaxation and how to maintain the ability of the pelvic floor muscles to be in a relaxed state throughout the day is taught as well.
Specific stretching and strengthening exercises are taught for the pelvic floor, the abdomen, and the pelvic girdle (the gluteal, hamstring, and adductor musculature).
Manual therapy such as soft tissue mobilization and trigger point release are administered to tight and restricted tissue both to the lower abdominal region and pelvic floor musculature to help increase blood flow, decrease restrictions, and promote healing. Education regarding normal bowel function and identification of problematic toileting habits is also an important step to recovery. By complying with a pelvic floor physical therapist’s recommendation, patients can be well on their way to pain-free and stress-free bowel function.
Cara Konlian, MSPT, is CEO of Aquacare Physical Therapy. She specializes in aquatic and pelvic floor physical therapy. Aquacare offers pelvic floor physical therapy for men and women and several of its 11 locations in Delaware and Maryland. To make an appointment, call the Aquacare location nearest you or schedule an appointment or evaluation online: www.aquacarephysicaltherapy.com.